Research Articles:
Cell Stress, Vol. 2, No. 11, pp. 311 - 324; doi: 10.15698/cst2018.11.163
p38β MAPK mediates ULK1-dependent induction of autophagy in skeletal muscle of tumor-bearing mice
1 Department of Integrative Biology and Pharmacology, McGovern Medical School, University of Texas Health Science Center, Houston, Texas 77030, USA.
2 Division of Endocrinology, Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China.
3 Department of Respiratory Medicine, Yixing Hospital affiliated to Jiangsu University, Yixing, China.
4 School of Public Health, University of Texas Health Science Center, Houston, Texas 77030, USA.
† These authors contributed equally.
# Yahui Wei and Yiman Wang were medical students of Jiaotong University, Shanghai, China participating in the Summer Research Program at McGovern Medical School, University of Texas Health Science Center at Houston.
Keywords: cachexia, muscle wasting, C/EBPβ, LC3b, Gabarapl1, ULK1.
Abbreviations:
AMPK – AMP-activated Protein Kinase,
C/EBPβ – CCAAT/enhancer-binding protein beta,
GFP – Green fluorescence protein,
HSP – Heat Shock Protein,
IL-6 – Interleukin 6
LCM – LLC Conditioned Medium,
LLC – Lewis Lung Carcinoma,
MAPK – Mitogen-Activated Protein Kinase,
MKO – Muscle specific Knock Out,
TA – Tibialis Anterior,
TLR4 – Toll-Like Receptor 4,
ULK1 – Unc-51 Like autophagy activating Kinase 1,
UPP – Ubiquitin-Proteasome Pathway.
Received originally: 22/06/2018 Received in revised form: 10/09/2018
Accepted: 24/10/2018
Published: 10/10/2018
Correspondence:
Yi-Ping Li, Department of Integrative Biology and Pharmacology, The University of Texas Health Science Center at Houston, 6431 Fannin Street, Houston, Texas 77030, USA. ORCID ID: orcid.org/0000-0002-0811-2790. Tel: (713) 500-6498, Fax: (713) 500-0689 yi-ping.li@uth.tmc.edu
Guohua Zhang, Department of Integrative Biology and Pharmacology, The University of Texas Health Science Center at Houston, 6431 Fannin Street, Houston, Texas 77030, USA. Tel: (713) 500-6322, Fax: (713) 500-0689 guohua.zhang@uth.tmc.edu
Conflict of interest statement: The authors declare that they have no conflict of interest.
Please cite this article as: Zhelong Liu, Ka Wai Thomas Sin, Hui Ding, HoangAnh Amy Doan, Song Gao, Hongyu Miao, Yahui Wei, Yiman Wang, Guohua Zhang, and Yi-Ping Li (2018). p38β MAPK mediates ULK1-dependent induction of autophagy in skeletal muscle of tumor-bearing mice. Cell Stress 2(11): 311-324. doi: 10.15698/cst2018.11.163
Abstract
Muscle wasting is the key manifestation of cancer-associated cachexia, a lethal metabolic disorder seen in over 50% of cancer patients. Autophagy is activated in cachectic muscle of cancer hosts along with the ubiquitin-proteasome pathway (UPP), contributing to accelerated protein degradation and muscle wasting. However, established signaling mechanism that activates autophagy in response to fasting or denervation does not seem to mediate cancer-provoked autophagy in skeletal myocytes. Here, we show that p38β MAPK mediates autophagy activation in cachectic muscle of tumor-bearing mice via novel mechanisms. Complementary genetic and pharmacological manipulations reveal that activation of p38β MAPK, but not p38α MAPK, is necessary and sufficient for Lewis lung carcinoma (LLC)-induced autophagy activation in skeletal muscle cells. Particularly, muscle-specific knockout of p38β MAPK abrogates LLC tumor-induced activation of autophagy and UPP, sparing tumor-bearing mice from muscle wasting. Mechanistically, p38β MAPK-mediated activation of transcription factor C/EBPβ is required for LLC-induced autophagy activation, and upregulation of autophagy-related genes LC3b and Gabarapl1. Surprisingly, ULK1 activation (phosphorylation at S555) by cancer requires p38β MAPK, rather than AMPK. Activated ULK1 forms a complex with p38β MAPK in myocytes, which is markedly increased by a tumor burden. Overexpression of a constitutively active p38β MAPK in HEK293 cells increases phosphorylation at S555 and other amino acid residues of ULK1, but not several of AMPK-mediated sites. Finally, ULK1 activation is abrogated in tumor-bearing mice with muscle-specific knockout of p38β MAPK. Thus, p38β MAPK appears a key mediator of cancer-provoked autophagy activation, and a therapeutic target of cancer-induced muscle wasting.
INTRODUCTION
Cancer has been increasingly recognized as a systemic disorder that stresses multiple organs independent of its location. At least 50% of cancer patients experience cachexia, a systemic wasting syndrome manifested as weight loss, inflammation, insulin resistance, and increased muscle protein breakdown. Progressive loss of muscle mass (muscle wasting) contributes significantly to cancer-associated morbidity and mortality [1][2]. However, the etiology of cancer cachexia is not well defined and there is no FDA-approved treatment for this lethal disorder.
–
There has been a general consensus that accelerated muscle protein degradation is a major cause of cachexia-associated muscle mass loss. It has been well-established that the ubiquitin proteasome pathway (UPP) plays an important role in cancer-induced muscle wasting by degrading myofibrillar proteins [3][4][5]. More recent evidence indicates that cancer also induces autophagy activation in the cachectic muscle of tumor-bearing mice [6][7][8][9] and cancer patients [10][11][12]. Autophagy targets cytoplasmic constituents including ubiquitinated protein aggregates and organelles for degradation by lysosomes [13][14]. Autophagy inhibition blocks muscle protein degradation induced by the activation of Toll-like receptor 4 (TLR4) [15], a plasma membrane receptor that is activated by danger-associated molecular patterns (DAMPs)[16] and mediates cancer-induced muscle wasting [4][9][17]. Thus, cancer-provoked autophagy activation is considered a therapeutic target of cancer-induced muscle wasting. However, the intramuscular signaling pathways that mediate cancer-induced activation of autophagy remain poorly understood. Elucidating and thereby targeting the cellular signaling pathways that mediate cancer-induced activation of autophagy could allow intervention of cancer-induced muscle wasting.
–
The Akt-FoxO signaling pathway inversely mediates the activity of both autophagy and UPP in muscle in response to such catabolic stimuli as fasting or denervation [18][19]. However, Akt is activated in cachectic muscle of tumor-bearing mice [20][21] and cancer patients [11][12], which inhibits FoxOs by promoting their translocation out of nuclei [22]. Thus, the Akt-FoxO signaling pathway does not appear to mediate cancer-induced muscle catabolism that is due largely to systemic inflammation. On the other hand, we observed previously that inflammation activated-p38 MAPK mediates both the autophagy and UPP activation in skeletal muscle in response to TLR4 activation by lipopolysaccharide [15]. Other inflammatory mediators implicated in cancer cachexia also activate p38 MAPK including oxidative stress [23], TNFα [24], IL-6 [25], IL-1 [26], TWEAK [27], activin A/myostatin [28] as well as extracellular Hsp70 and Hsp90 [4], while promoting autophagy and/or UPP-mediated muscle protein loss. However, it is unknown which of the three p38 MAPK isoforms that are expressed in skeletal muscle (a, b, and g) mediates cancer-induced autophagy activation. More importantly, how p38 MAPK activates autophagy is unknown.
–
In the present study, we demonstrate that activation of the p38β MAPK isoform is necessary and sufficient for autophagy activation in skeletal muscle in a mouse model of cancer cachexia, and that deletion of p38β MAPK in skeletal muscle abrogates muscle wasting by attenuating muscle protein degradation mediated by autophagy as well as UPP. Mechanistically, p38β MAPK mediates cancer-provoked autophagy activation by upregulating Atg8 orthologues LC3b and Gabarapl1 as well as by activating ULK1. These data support p38β MAPK as a key mediator and therapeutic target of cancer-associated muscle wasting.
RESULTS
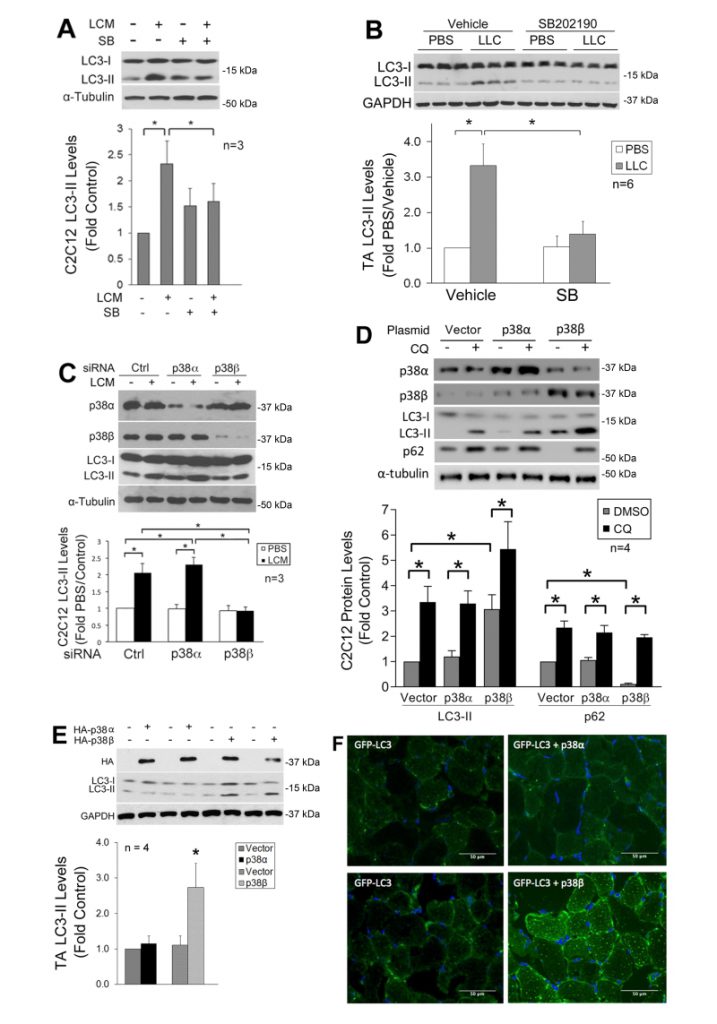
LLC induces autophagy activation in skeletal muscle cells through p38β MAPK
We previously showed that LLC induces an increase in autophagy flux and autophagosome formation in cultured C2C12 myotubes as well as mouse muscle [9]. In the present study, we further investigated whether LLC induces autophagy activation in skeletal muscle cells through p38 MAPK by monitoring the autophagy marker LC3-II. By pretreating C2C12 myotubes, which respond to cancer cell-conditioned media in a similar manner as primary myotubes [4], with a p38α/β MAPK inhibitor SB202190, we observed that the induction of autophagy by LLC cell-conditioned medium (LCM) required p38 MAPK activation (Figure 1A). In addition, systemic administration of SB202190 to LLC tumor-bearing mice inhibited autophagy activation in cachectic muscle (Figure 1B). These results suggest that LLC induces autophagy activation in skeletal muscle through the activation of p38α and/or p38β MAPK.
–
–
To identify the isoform of p38 MAPK that mediated LLC induction of autophagy, we utilized siRNA-mediated gene silencing and observed that the loss of p38β MAPK, but not p38α MAPK, abolished LCM-induced autophagy activation (Figure 1C). To examine whether activated p38β MAPK actually stimulated autophagy flux, a constitutively active mutant of p38α MAPK or p38β MAPK [29] was expressed in myotubes. Only the active p38β MAPK increased the LC3-II level. In addition, treatment of myotubes with lysosome inhibitor chloroquine (CQ) further increased LC3-II in active p38β MAPK-expressing myotubes. Further, expression of active p38β MAPK resulted in a loss in the autophagy-selective target p62, and CQ treatment abrogated this effect (Figure 1D). These results indicate that p38β MAPK activation stimulated autophagy flux. Similarly, LC3-II was specifically increased by the overexpressed active mutant of p38β MAPK in the muscle (TA) of tumor-free mice (Figure 1E). Furthermore, co-transfection of GFP-LC3 with active p38β MAPK, but not active p38α MAPK, in mouse muscle resulted in increased autophagosome formation as indicated by the formation of GFP-LC3-incorporated puncta (Figure 1F). These data provided evidence that p38β MAPK activation is necessary and sufficient for autophagy activation in skeletal muscle cells by a tumor burden.
–
–
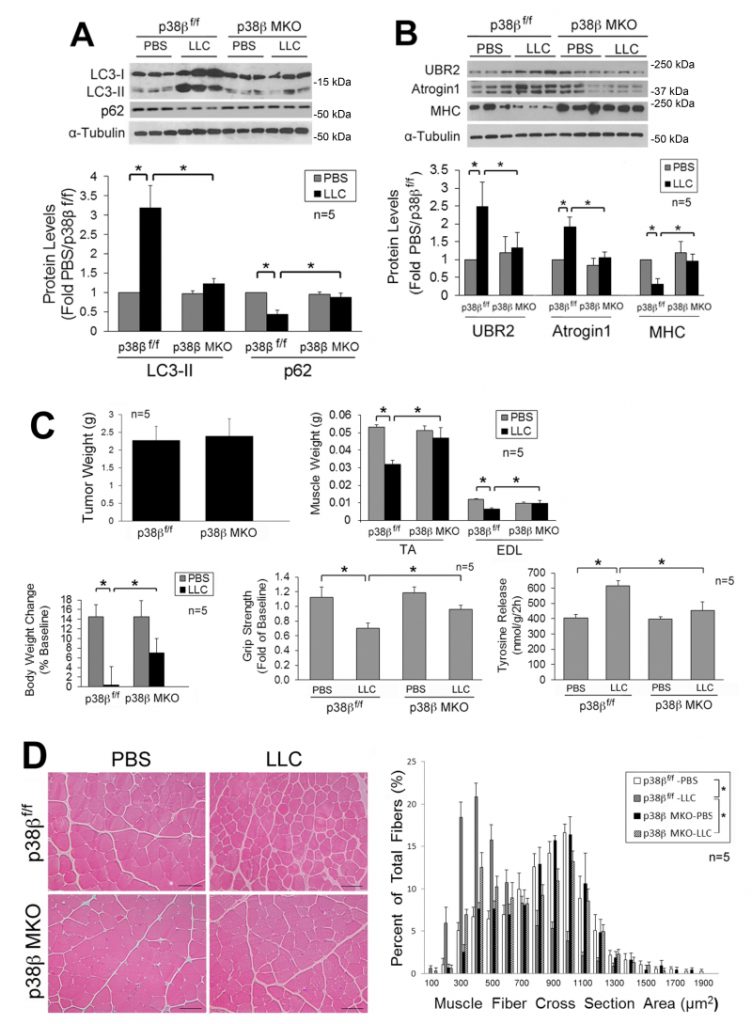
LLC induces muscle wasting through p38β MAPK-mediated activation of autophagy and UPP
Next, we investigated whether LLC-induced activation of autophagy and muscle wasting are attenuated in the muscle of mice with muscle-specific knockout of p38β MAPK (p38β MKO) [30]. It was previously shown that the muscle phenotype was not altered by deleting the p38β gene [28][30][31]. We observed that p38β MKO mice were resistant to LLC-induced autophagy activation as measured by LC3-II and p62 levels (Figure 2A). In addition, p38β MKO mice were resistant to LLC-stimulated UPP activity as monitored by the levels of atrogin1, UBR2 and myofibrillar protein myosin heavy chain (MHC) (Figure 2B). Consequently, p38β MKO mice were spared from LLC-induced muscle wasting without altering tumor growth as measured by tumor weight, body and muscle weight, muscle proteolysis (tyrosine release), muscle strength (grip strength, Figure 2C) and myofiber cross-sectional area (Figure 2D). Thus, LLC induces muscle wasting through p38β MAPK-mediated activation of both autophagy and UPP.
–
–
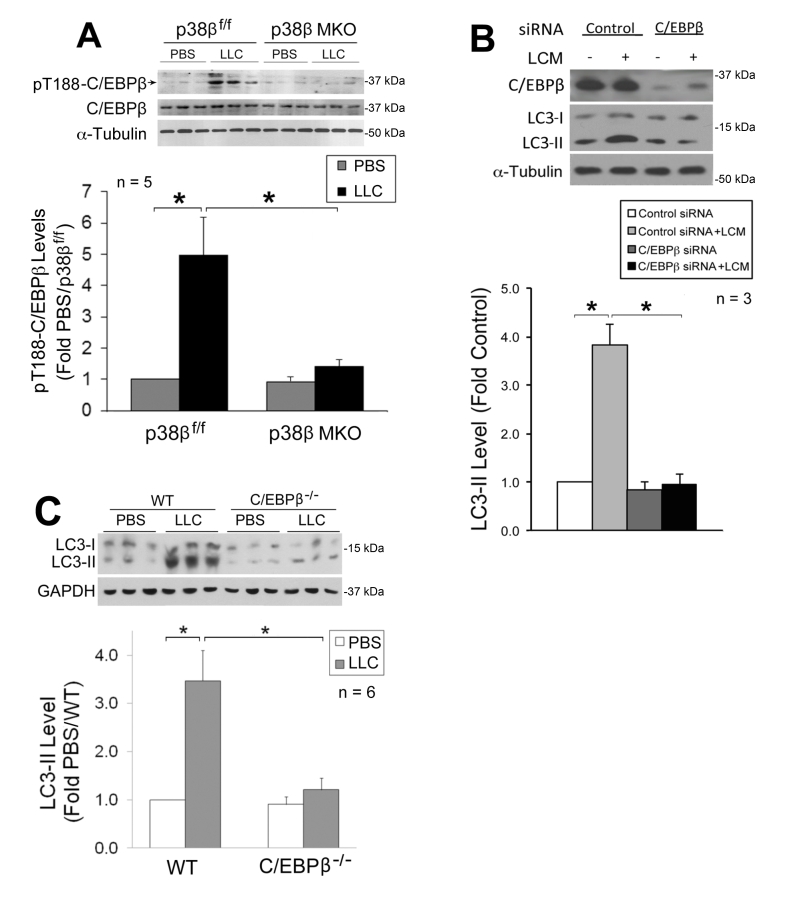
p38β MAPK-mediated C/EBPβ activation is critical to LLC-induced autophagy activation
We previously showed that p38β MAPK mediates LLC-induced upregulation of atrogin1 [29] and UBR2 [32] through the activation of C/EBPβ-binding to a cis-element in their 5’-promoter by phosphorylating the Thr-188 residue of C/EBPβ [29], and that LLC-induced muscle wasting is abrogated in C/EBPβ knockout mice [21]. We therefore investigated whether the p38β MAPK → C/EBPβ signaling pathway also mediates LLC activation of autophagy. We observed that LLC-induced activation of C/EBPβ was blocked in the muscle of p38β MKO mice (Figure 3A), confirming in vivo that p38β MAPK mediates LLC-induced activation of C/EBPβ. To investigate whether C/EBPβ is critical to LLC-induced autophagy activation, we treated C/EBPβ-deficient C2C12 myotubes with LCM, and observed a dependence of LCM-induced autophagy activation on C/EBPβ (Figure 3B). Further, we observed that LLC-induced autophagy activation was abrogated in the muscle of C/EBPβ knockout mice (Figure 3C). Thus, p38β MAPK-mediated activation of C/EBPβ is critical to LLC-induced autophagy activation.
–
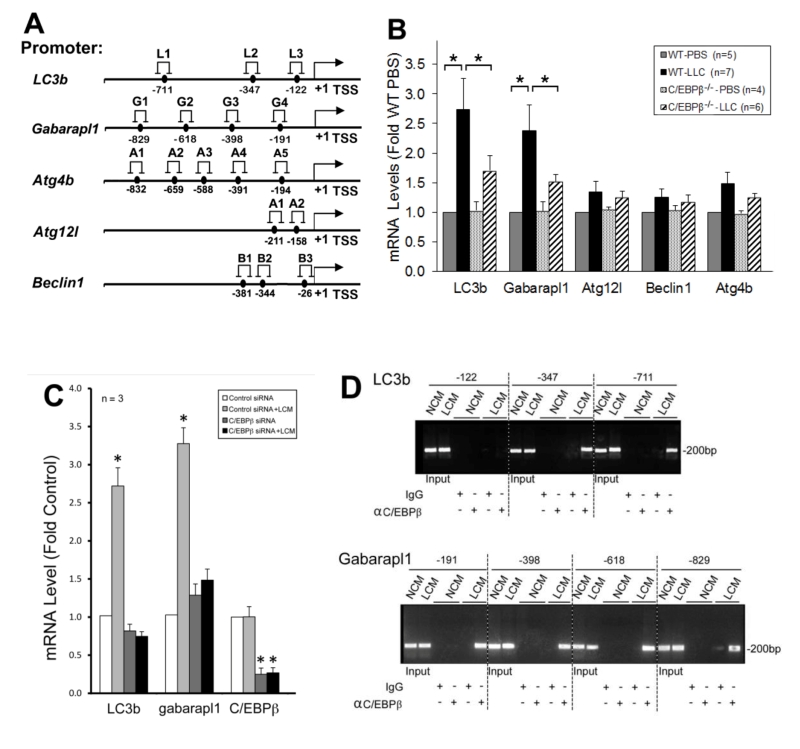
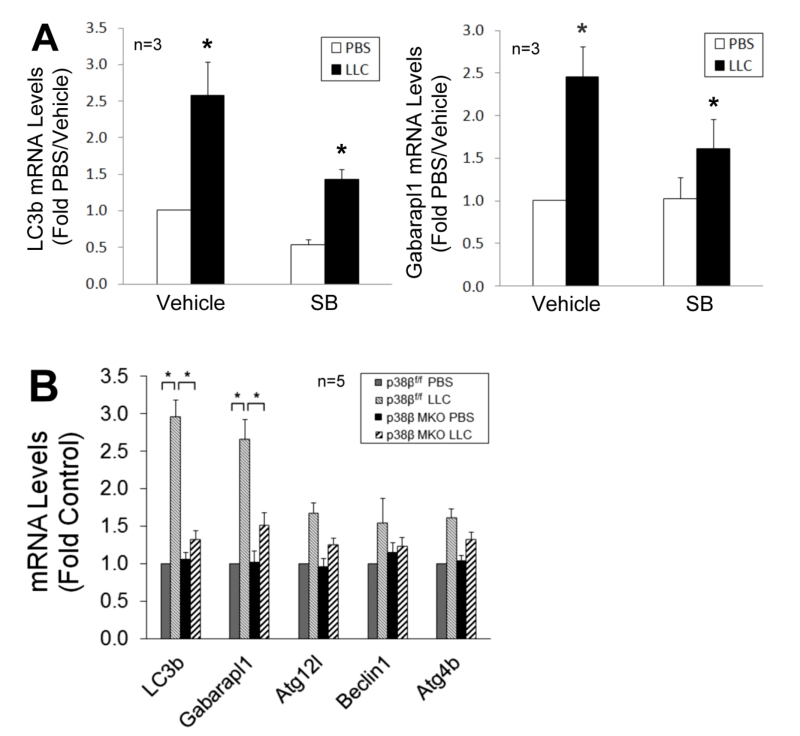
p38β MAPK → C/EBPβ signaling mediates upregulation of specific autophagy-related genes
To understand how C/EBPβ mediates LLC-induced autophagy activation, we searched a data base (http://tfbind.hgc.jp/) for potential C/EBPβ-binding sites in the 5’-promoter regions of autophagy-related genes and identified multiple sites within –1 kilo-bases in five important autophagy related genes (Figure 4A). By analyzing mRNA levels of these genes in the muscle of LLC tumor-bearing wild type and C/EBPβ knockout mice, we found that mRNA of LC3b and Gabarapl1, two Atg8 orthologues, were upregulated by LLC in a C/EBPβ-dependent manner (Figure 4B). Corroborative data were obtained in C2C12 myotubes where LCM treatment upregulated the two genes in a C/EBPβ-dependent manner (Figure 4C). To determine whether LLC stimulates C/EBPβ binding to the two gene promoters, we performed the chromatin immunoprecipitation (ChIP) assay and observed that LCM treatment of C2C12 myotubes stimulated C/EBPβ binding to multiple sites in the LC3b and Gabarapl1 promoter (Figure 4D). These data suggest that C/EBPβ upregulates the two Atg8 orthologues in muscle cells in response to a tumor burden.
–
–
To verify whether p38β MAPK is required for C/EBPβ-mediated upregulation of LC3b and Gabarapl1, we observed that the upregulation of these genes in LCM-treated myotubes was inhibited by SB202190 (Figure 5A). Further, upregulation of these genes in skeletal muscle was abrogated in LLC tumor–bearing p38β MKO mice (Figure 5B). These data confirm that LLC upregulates LC3b and Gabarapl1 through the p38β MAPK → C/EBPβ signaling pathway.
–
–
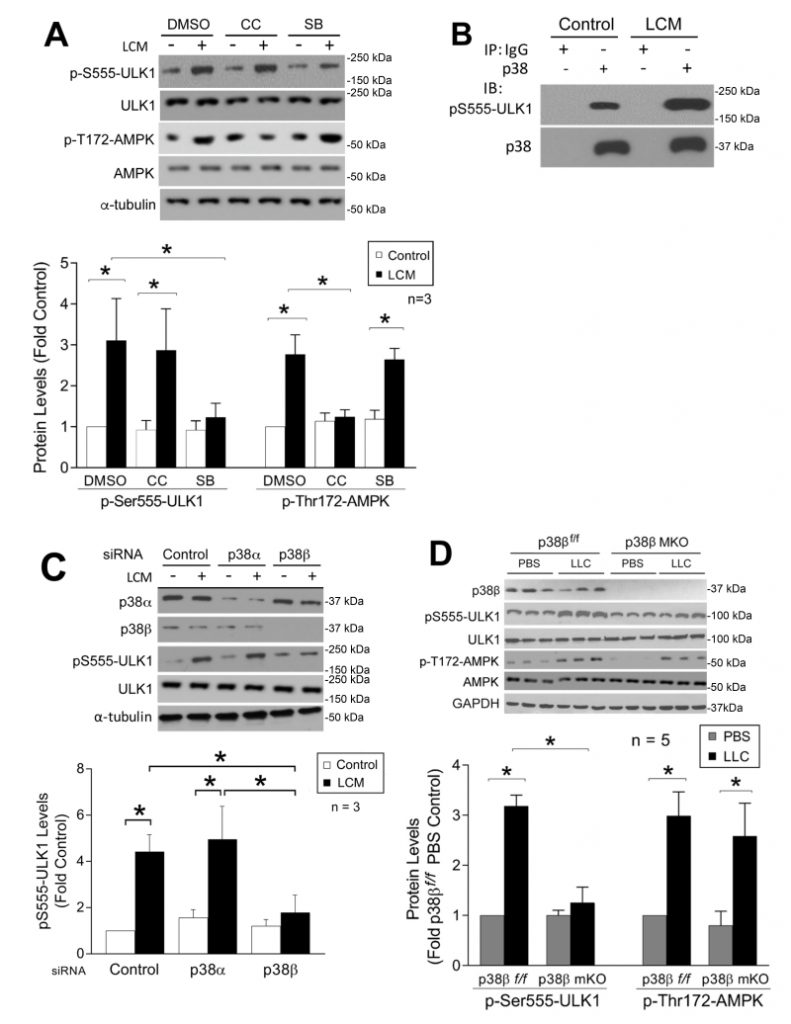
LLC induces ULK1 activation in skeletal muscle through p38β MAPK
Both LC3b and Gabarapl1 are members of the ATG8 family that are essential for autophagosome formation [33]. On the other hand, ATG8 family members must be activated by the ULK1 complex post-translationally to initiate the lipidation process required for autophagsome formation [34]. Therefore, we examined whether LLC induced ULK1 activation in skeletal muscle cells. LCM treatment of C2C12 myotubes for 1 h increased ULK1 phosphorylation on Ser-555 (pS555-ULK1, Figure 6A). Phosphorylation of ULK1 on this serine residue is known to activate ULK1 by AMP-activated protein kinase (AMPK) upon nutrient deprivation [35][36]. LCM was shown previously to induce mTOR inhibition and AMPK activation in C2C12 myotubes [37]. To examine the involvement of AMPK in LCM-induced activation of ULK1, we pretreated myotubes with the AMPK inhibitor Compound C [38]. To our surprise, Compound C did not alter LCM-induced ULK1 phosphorylation on Ser-555, although it did inhibit AMPK activation as measured by the phosphorylation state of its Thr-172 residue. However, pretreatment with p38 MAPK inhibitor SB202190 attenuated LCM-induced Ser-555 phosphorylation of ULK-1, without affecting LCM-induced Thr-172 phosphorylation of AMPK (Figure 6A). These data suggest that p38 MAPK, rather than AMPK, is critical to LCM-induced activation of ULK1. We then investigated whether p38 MAPK interacted with ULK1 by performing immunoprecipitation of p38 MAPK from myotube lysate. We observed co-precipitation of pS555-ULK1 with p38 MAPK in control myotubes, and that the level of co-precipitated pS555-ULK1 dramatically increased in LCM-treated myotubes (Figure 6B), suggesting that p38 MAPK does interact with ULK1 resulting in phosphorylation of its Ser-555 residue in myocytes, and this activity is stimulated upon p38 MAPK activation by a tumor burden. To identify the p38 MAPK isoform responsible for LCM-stimulated ULK1 phosphorylation on Ser-555, we performed siRNA-mediated gene silencing in myotubes and observed that p38β MAPK, but not p38α MAPK, was required for this reaction (Figure 6C). To verify that activation of p38β MAPK is sufficient to phosphorylate ULK1, FLAG-tagged ULK1 was co-expressed with constitutively active p38β MAPK in HEK293T cells. Mass spectrometry analysis of FLAG-ULK1 isolated from cell lysate revealed multiple phosphorylated amino acid residues including Ser-555 (Supplementary Table 1). However, these sites did not include a number of known AMPK-mediated phosphorylation sites in ULK1 such as Ser-317, Ser-467, Ser-637 and Ser-777 [36][39]. In combination, the above data support that p38β MAPK stimulates ULK1 activity upon activation by cancer independent of AMPK in the cellular environment. Finally, we confirmed that Ser-555 phosphorylation of ULK1 increased in the muscle of LLC tumor-bearing p38βf/f mice but not in that of muscle-specific p38β MAPK knockout mice. On the other hand, LLC-induced AMPK activation was not altered in p38β MAPK-deficient muscle (Figure 6E). Therefore, we conclude that p38β MAPK, rather than AMPK, mediates LLC-induced autophagosome formation by activating ULK1 in addition to upregulating LC3b and Gabarapl1.
–
DISCUSSION
The current study identifies p38β MAPK as a key mediator of cancer-induced autophagy activation in skeletal muscle, through activating ULK1 as well as upregulating C/EBPβ-controlled LC3b and Gabarapl1 genes. Importantly, we were able to abrogate cancer-induced muscle wasting by deleting p38β MAPK in skeletal muscle to prevent muscle protein degradation mediated by autophagy as well as UPP. These findings suggest that p38β MAPK is a key mediator and a therapeutic target of cancer-induced muscle wasting.
–
We show that p38β MAPK upregulates LC3b and Gabarapl1 through activating C/EBPβ. The LC3 and Gabarapl family of proteins are mammalian orthologues of ATG8, a yeast autophagy-related protein involved in the formation of autophagosomes [33]. Increased expression of LC3/Gabaraple and activation of autophagy have been observed in cachectic muscle of cancer patients [10][11][12]. In various types of cells, increased expression of LC3/Gabarapl are often associated with autophagy activation [40][41]. As the substrates of ULK1-mediated lipidation process that is critical for autophagosome formation [34], increased expression of LC3/Gabarapl is likely to facilitate autophagosome formation. On the other hand, the possibility exists that C/EBPβ may regulate additional autophagy-related genes that are rate-limiting for autophagosome formation.
–
Autophagy is activated by nutritional deprivation through AMPK-mediated phosphorylation of ULK1 on multiple sites including Ser-555 in various cell types [35][36]. In skeletal muscle, autophagy is also activated by the inactivation of Akt that inversely regulates FoxO3-mediated upregulation of autophagy-related gene expression in response to denervation or starvation [18][42], or by AMPK-mediated activation of FoxO3 in response to C26 colon adenocarcinoma [43]. We previously showed that LLC activates Akt and inactivates FoxO1/3 in muscle cells, while activating p38 MAPK concomitantly [21]. In the present study we show that despite AMPK activation by LLC in skeletal muscle, AMPK does not mediate in ULK1 activation LLC tumor-bearing mice. On the contrary, autophagy activation in skeletal muscle by LLC requires p38β MAPK-mediated activation of ULK1. Thus, tumor activates autophagy in skeletal muscle through a signaling mechanism distinct from that in nutritional deprivation.
–
It is well-established that in skeletal muscle p38 MAPK is activated by various inflammatory mediators implicated in cancer cachexia including various cytokines [24][25][26][27][28], reactive oxygen species (ROS)[23] and extracellular vesicle-associated Hsp70 and Hsp90 [4]. Of the three members of p38 MAPK family expressed in skeletal muscle, p38α MAPK is responsible for most of the known roles of p38 MAPK including mediating inflammation [44][45] and promoting myogenesis [46][47]. p38γ MAPK regulates the expansion of myogenic precursor cells [48], endurance exercise-induced mitochondrial biogenesis and angiogenesis [30], as well as glucose uptake [49]. On the other hand, p38β MAPK has few known functions. Utilizing genetic manipulations including the p38β MAPK muscle specific knockout mice [30] in addition to pharmacological inhibition of p38α/β MAPK (due to the lack of p38β MAPK-specific inhibitors), the current study demonstrated for the first time that p38β MAPK is essential to autophagy activation during muscle wasting induced by LLC. The current study also demonstrated for the first time in vivo that p38β MAPK is essential to UPP activation and muscle wasting induced by cancer. Therefore, developing p38β MAPK-specific pharmacological inhibitors would be highly desirable for the intervention of cancer cachexia.
–
Our findings on the role of p38β MAPK in autophagy activation may have significance beyond skeletal muscle cells. For example, p38 MAPK mediates various stress-induced autophagy activation in a variety of cells [50][51][52][53][54]. Particularly, in response to TLR4 activation, p38 MAPK mediates autophagy activation associated with innate immunity [55], which is similar to cancer-induced muscle wasting [4][9][17]. However, which p38 MAPK isoform and how it activates autophagy in those processes are unknown. It is possible that a similar mechanism as we observed in skeletal muscle cells exists in other types of cells to mediate autophagy activation in response to inflammatory stresses.
–
Taken together, our findings reveal that p38β MAPK mediates cancer-induced autophagy in skeletal muscle through novel transcriptional as well as post-translational mechanisms. In addition, our findings suggest that cancer-induced muscle wasting can be ameliorated by targeting a single signaling molecule in skeletal muscle, p38β MAPK.
MATERIALS AND METHODS
Myogenic cell culture
Murine C2C12 myoblasts (American Type Culture Collection) were cultured in growth medium (DMEM supplemented with 10% fetal bovine serum) at 37°C with 5% CO2. At 85–90% confluence, myoblast differentiation was induced by incubation for 96 h in differentiation medium (DMEM supplemented with 4% heat-inactivated horse serum) to form myotubes. Preconditioned medium from cultures of Lewis lung carcinoma cells (obtained from National Institute of Cancer, Frederick, MD) or non-tumorigenic human lung epithelial cell line NL20 (obtained from American Type Culture Collection) that were cultured for 48 h were centrifuged and the supernatant was used to treat C2C12 myotubes (25% final volume in fresh medium) when indicated. Pretreatment of SB202190 or compound C (10 μM, dissolved in DMSO with 0.1% final concentration, Sigma-Aldrich, St. Louis, MO) for 30 min was carried out when indicated. All cell culture experiments were independently replicated 3 times as indicated (N = 3).
–
Animal use
Experimental protocols were approved in advance by the institutional Animal Welfare Committee at the University of Texas Health Science Center at Houston. For LLC cell xenograft, 100 ml LLC (National Institute of Cancer) cells (1 × 106 cells), or an equal volume of vehicle (PBS) was injected subcutaneously into the right flanks of 7-week-old male C57BL/6 mice (The Jackson Laboratory, Bar Harbor, ME), C/EBPβ-/- mice in C57BL/6 background that were bred from C/EBPβ-/+ mice [56] or mice with muscle-specific knockout of p38β (p38β MKO) [28]. The latter were created by crossbreeding floxed-p38β mice (p38β f/f) in C57BL/6 background [30] with muscle creatine kinase-Cre (MCK-Cre, The Jackson Laboratory, Bar Harbor, ME). SB202190 was i.p. injected (5 mg/kg) daily from day 7 of tumor implant. Mice were euthanized on day 21 for evaluation of muscle wasting. When indicated plasmids encoding constitutively active mutant of p38 MAPK isoforms and GFP-LC3 fusion protein [55] were transfected into TA by electroporation as previously described [29].
–
Transfection of siRNA and plasmids in C2C12 myoblasts
Predesigned siRNAs specific for C/EBPβ, p38α and p38β were purchased form Sigma-Aldrich. The IDs of the siRNAs were SASI_Mm01_00187563, SASI_Mm01_00020743 and SASI_Mm01_00044863, respectively. Control siRNA was purchased from Invitrogen. These siRNAs were introduced into C2C12 myoblasts using the jetPRIME reagent (Polyplus-transfection Inc., Illkirch, France) according to the manufacturer’s protocol. In 24 h, myoblasts were differentiated and experiments were started in another 96 h when myotubes were formed. Plasmids encoding constitutively active p38α and p38β isoforms [57] were transfected into C2C12 myoblasts using the jetPRIME reagent. Empty vector was transfected as the control. These manipulation of p38 MAPK in myoblasts did not alter the end result of differentiation and formation of myotubes [29].
–
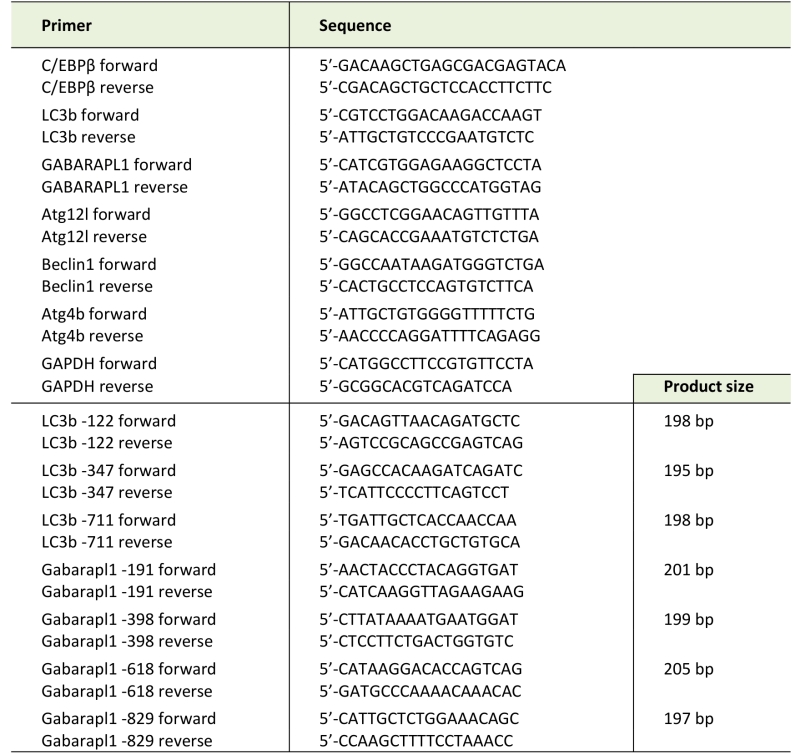
Real-time PCR
Total RNA was isolated from myotubes or muscle by using TRIzol reagent (Invitrogen, Carlsbad, CA). Real-time PCR was performed as described previously [21]. Sequences of specific primers are listed in Table 1. Data were normalized to GAPDH.
–
TABLE 1. PCR primers used in this study. |
 |
–
Western blot analysis
Western blot analysis was carried out as described previously [24]. Antibodies to total and/or phosphorylated p38MAPK (T181/Y182), p-C/EBPβ (T188), p-ULK1 (S555), total and phosphorylated AMPK (T172), p62 as well as p38α and p38β were from Cell Signaling Technology (Beverly, MA). Antibody to C/EBPβ and ULK1 were from Santa Cruz Biotechnology (Santa Cruz, CA). Antibody to atrogin1/MAFbx was from ECM Biosciences (Versailles, KY). Antibodies to UBR2 and LC3-II were obtained from Novus Biologicals (Littleton, CO). Anti-MHC antibody (MF-20) was from R&D Systems (Minneapolis, MN). Antibody to the HA tag was from Covance (Princeton, NJ, USA). Data was normalized to α-Tubulin (antibody was from Development Studies Hybridoma Bank at the University of Iowa, Iowa City, IA) or GAPDH (Antibody was from Millipore, Billerica, MA, USA). Levels of phosphorylated proteins were normalized to corresponding total proteins.
–
Chromosome immunoprecipitation (ChIP) assay
ChIP assay was performed as previously described [21]. Antibody against C/EBPβ was from Santa Cruz Biotechnology. Pre-immune IgG was from Sigma-Aldrich. The PCR primers used are listed in Table 1.
–
Histology and confocal microscopy studies
Cross sections of TA were fixed and stained with H&E by the Histology Core at Lester and Sue Smith Breast Center, Baylor College of Medicine. Cross-sectional area of stained muscle sections was quantified by using the ImageJ software (NIH). Five view-fields with ~100 myofibers per field in each section were measured. Frozen sections of mouse TA (5 mm) that expressed GFP-LC3 and/or p38 MAPK mutant were stained with DAPI and examined with a Nikon A1R Confocal Laser Microscope using 60X objective.
–
Adjustment of brightness, contrast, color balance, and final image size was achieved using Adobe Photoshop CS (Adobe Systems, San Jose, CA, USA).
–
Mapping of phosphorylated amino acid residues in ULK-1
HEK293T cells (American Type Culture Collection, Manassas, VA, USA) cultured in 150 mm plates that were ~50% confluent were co-transfected with a plasmid encoding mouse ULK-1 with a FLAG tag (Addgene) and a plasmid encoding constitutively active p38β [58] (10 μg each) using the jetPRIME reagent (Polyplus-transfection Inc., Illkirch, France). The cell culture medium was replaced with fresh medium at 24 h. After an additional incubation of 24 h cells were lysed in RIPA buffer (50 mM Tris– HCl (pH 7.5), 150 mM NaCl, 2 mM EDTA, 1% NP-40, 0.1% SDS, 2 mM phenylmethylsulphonylfluoride (PMSF), 0.5% sodium deoxycholate, 1 mM NaF, 1/100 protease inhibitor cocktail, and 1/100 phosphatase inhibitor cocktail (Sigma-Aldrich, St. Louis, MO, USA). ULK-1 in cell lysates was precipitated using FLAG-M2 magnetic beads (Sigma-Aldrich) and subjected to 10% SDS-PAGE. The gel was then stained with Coommassie Blue R-250. The ULK1 band was cut out and subjected to tryptic phosphopeptide mapping conducted by Taplin Mass Spectrometry Facility at Harvard Medical School using an LTQ-Orbitrap mass spectrometer (Thermo Electron, West Palm Beach, FL, USA).
–
Statistical analysis
Data are presented as the mean ± S.D. and were analyzed with one-way ANOVA or Student t test using the SigmaStat software (Systat Software, San Jose, CA) as indicated. When applicable, control samples from independent experiments were normalized to a value of 1 without showing variations (actual variations were within a normal range). Chi-square analysis was carried out by using R to compare the distributions of muscle fiber cross-sectional area among various groups. A p value < 0.05 was considered to be statistically significant.
References
- K. Fearon, F. Strasser, S.D. Anker, I. Bosaeus, E. Bruera, R.L. Fainsinger, A. Jatoi, C. Loprinzi, N. MacDonald, G. Mantovani, M. Davis, M. Muscaritoli, F. Ottery, L. Radbruch, P. Ravasco, D. Walsh, A. Wilcock, S. Kaasa, and V.E. Baracos, "Definition and classification of cancer cachexia: an international consensus", The Lancet Oncology, vol. 12, pp. 489-495, 2011. http://dx.doi.org/10.1016/S1470-2045(10)70218-7
- K. Fearon, D. Glass, and D. Guttridge, "Cancer Cachexia: Mediators, Signaling, and Metabolic Pathways", Cell Metabolism, vol. 16, pp. 153-166, 2012. http://dx.doi.org/10.1016/j.cmet.2012.06.011
- S.H. Lecker, R.T. Jagoe, A. Gilbert, M. Gomes, V. Baracos, J. Bailey, S.R. Price, W.E. Mitch, and A.L. Goldberg, "Multiple types of skeletal muscle atrophy involve a common program of changes in gene expression", The FASEB Journal, vol. 18, pp. 39-51, 2004. http://dx.doi.org/10.1096/fj.03-0610com
- G. Zhang, Z. Liu, H. Ding, Y. Zhou, H.A. Doan, K.W.T. Sin, Z.J. Zhu, R. Flores, Y. Wen, X. Gong, Q. Liu, and Y. Li, "Tumor induces muscle wasting in mice through releasing extracellular Hsp70 and Hsp90", Nature Communications, vol. 8, 2017. http://dx.doi.org/10.1038/s41467-017-00726-x
- X. Zhou, J.L. Wang, J. Lu, Y. Song, K.S. Kwak, Q. Jiao, R. Rosenfeld, Q. Chen, T. Boone, W.S. Simonet, D.L. Lacey, A.L. Goldberg, and H. Han, "Reversal of Cancer Cachexia and Muscle Wasting by ActRIIB Antagonism Leads to Prolonged Survival", Cell, vol. 142, pp. 531-543, 2010. http://dx.doi.org/10.1016/j.cell.2010.07.011
- F. Penna, D. Costamagna, F. Pin, A. Camperi, A. Fanzani, E.M. Chiarpotto, G. Cavallini, G. Bonelli, F.M. Baccino, and P. Costelli, "Autophagic Degradation Contributes to Muscle Wasting in Cancer Cachexia", The American Journal of Pathology, vol. 182, pp. 1367-1378, 2013. http://dx.doi.org/10.1016/j.ajpath.2012.12.023
- K.R. Bohnert, Y.S. Gallot, S. Sato, G. Xiong, S.M. Hindi, and A. Kumar, "Inhibition of ER stress and unfolding protein response pathways causes skeletal muscle wasting during cancer cachexia", The FASEB Journal, vol. 30, pp. 3053-3068, 2016. http://dx.doi.org/10.1096/fj.201600250RR
- E.E. Talbert, G.A. Metzger, W.A. He, and D.C. Guttridge, "Modeling human cancer cachexia in colon 26 tumor‐bearing adult mice", Journal of Cachexia, Sarcopenia and Muscle, vol. 5, pp. 321-328, 2014. http://dx.doi.org/10.1007/s13539-014-0141-2
- G. Zhang, Z. Liu, H. Ding, H. Miao, J.M. Garcia, and Y. Li, "Toll-like receptor 4 mediates Lewis lung carcinoma-induced muscle wasting via coordinate activation of protein degradation pathways", Scientific Reports, vol. 7, 2017. http://dx.doi.org/10.1038/s41598-017-02347-2
- Z. Aversa, F. Pin, S. Lucia, F. Penna, R. Verzaro, M. Fazi, G. Colasante, A. Tirone, F.R. Fanelli, C. Ramaccini, P. Costelli, and M. Muscaritoli, "Autophagy is induced in the skeletal muscle of cachectic cancer patients", Scientific Reports, vol. 6, 2016. http://dx.doi.org/10.1038/srep30340
- N.A. Stephens, R.J.E. Skipworth, I.J. Gallagher, C.A. Greig, D.C. Guttridge, J.A. Ross, and K.C.H. Fearon, "Evaluating potential biomarkers of cachexia and survival in skeletal muscle of upper gastrointestinal cancer patients", Journal of Cachexia, Sarcopenia and Muscle, vol. 6, pp. 53-61, 2015. http://dx.doi.org/10.1002/jcsm.12005
- C.M. Op den Kamp, R.C. Langen, F.J. Snepvangers, C.C. de Theije, J.M. Schellekens, F. Laugs, A.C. Dingemans, and A.M. Schols, "Nuclear transcription factor κ B activation and protein turnover adaptations in skeletal muscle of patients with progressive stages of lung cancer cachexia", The American Journal of Clinical Nutrition, vol. 98, pp. 738-748, 2013. http://dx.doi.org/10.3945/ajcn.113.058388
- D. Bechet, A. Tassa, D. Taillandier, L. Combaret, and D. Attaix, "Lysosomal proteolysis in skeletal muscle", The International Journal of Biochemistry & Cell Biology, vol. 37, pp. 2098-2114, 2005. http://dx.doi.org/10.1016/j.biocel.2005.02.029
- V. Kirkin, D.G. McEwan, I. Novak, and I. Dikic, "A Role for Ubiquitin in Selective Autophagy", Molecular Cell, vol. 34, pp. 259-269, 2009. http://dx.doi.org/10.1016/j.molcel.2009.04.026
- A. Doyle, G. Zhang, E.A.A. Fattah, N.T. Eissa, and Y. Li, "Toll‐like receptor 4 mediates lipopolysaccharide‐induced muscle catabolismviacoordinate activation of ubiquitin‐proteasome and autophagy‐lysosome pathways", The FASEB Journal, vol. 25, pp. 99-110, 2010. http://dx.doi.org/10.1096/fj.10-164152
- M.E. Bianchi, "DAMPs, PAMPs and alarmins: all we need to know about danger", Journal of Leukocyte Biology, vol. 81, pp. 1-5, 2006. http://dx.doi.org/10.1189/jlb.0306164
- T.Y. Cannon, D. Guttridge, J. Dahlman, J.R. George, V. Lai, C. Shores, P. Bužková, and M.E. Couch, "The Effect of Altered Toll-like Receptor 4 Signaling on Cancer Cachexia", Archives of Otolaryngology–Head & Neck Surgery, vol. 133, pp. 1263, 2007. http://dx.doi.org/10.1001/archotol.133.12.1263
- J. Zhao, J.J. Brault, A. Schild, P. Cao, M. Sandri, S. Schiaffino, S.H. Lecker, and A.L. Goldberg, "FoxO3 Coordinately Activates Protein Degradation by the Autophagic/Lysosomal and Proteasomal Pathways in Atrophying Muscle Cells", Cell Metabolism, vol. 6, pp. 472-483, 2007. http://dx.doi.org/10.1016/j.cmet.2007.11.004
- G. Milan, V. Romanello, F. Pescatore, A. Armani, J. Paik, L. Frasson, A. Seydel, J. Zhao, R. Abraham, A.L. Goldberg, B. Blaauw, R.A. DePinho, and M. Sandri, "Regulation of autophagy and the ubiquitin–proteasome system by the FoxO transcriptional network during muscle atrophy", Nature Communications, vol. 6, 2015. http://dx.doi.org/10.1038/ncomms7670
- F. Penna, A. Bonetto, M. Muscaritoli, D. Costamagna, V.G. Minero, G. Bonelli, F.R. Fanelli, F.M. Baccino, and P. Costelli, "Muscle atrophy in experimental cancer cachexia: Is the IGF‐1 signaling pathway involved?", International Journal of Cancer, vol. 127, pp. 1706-1717, 2010. http://dx.doi.org/10.1002/ijc.25146
- G. Zhang, B. Jin, and Y. Li, "C/EBPβ mediates tumour-induced ubiquitin ligase atrogin1/MAFbx upregulation and muscle wasting", The EMBO Journal, vol. 30, pp. 4323-4335, 2011. http://dx.doi.org/10.1038/emboj.2011.292
- M. Sandri, C. Sandri, A. Gilbert, C. Skurk, E. Calabria, A. Picard, K. Walsh, S. Schiaffino, S.H. Lecker, and A.L. Goldberg, "Foxo Transcription Factors Induce the Atrophy-Related Ubiquitin Ligase Atrogin-1 and Cause Skeletal Muscle Atrophy", Cell, vol. 117, pp. 399-412, 2004. http://dx.doi.org/10.1016/s0092-8674(04)00400-3
- J.M. McClung, A.R. Judge, S.K. Powers, and Z. Yan, "p38 MAPK links oxidative stress to autophagy-related gene expression in cachectic muscle wasting", American Journal of Physiology-Cell Physiology, vol. 298, pp. C542-C549, 2010. http://dx.doi.org/10.1152/ajpcell.00192.2009
- Y. Li, Y. Chen, J. John, J. Moylan, B. Jin, D.L. Mann, and M.B. Reid, "TNF‐α acts via p38 MAPK to stimulate expression of the ubiquitin ligase atrogin1/MAFbx in skeletal muscle", The FASEB Journal, vol. 19, pp. 362-370, 2005. http://dx.doi.org/10.1096/fj.04-2364com
- M.J. Puppa, S. Gao, A.A. Narsale, and J.A. Carson, "Skeletal muscle glycoprotein 130's role in Lewis lung carcinoma–induced cachexia", The FASEB Journal, vol. 28, pp. 998-1009, 2013. http://dx.doi.org/10.1096/fj.13-240580
- W. Li, J.S. Moylan, M.A. Chambers, J. Smith, and M.B. Reid, "Interleukin-1 stimulates catabolism in C2C12 myotubes", American Journal of Physiology-Cell Physiology, vol. 297, pp. C706-C714, 2009. http://dx.doi.org/10.1152/ajpcell.00626.2008
- H. Li, A. Mittal, P.K. Paul, M. Kumar, D.S. Srivastava, S.C. Tyagi, and A. Kumar, "Tumor Necrosis Factor-related Weak Inducer of Apoptosis Augments Matrix Metalloproteinase 9 (MMP-9) Production in Skeletal Muscle through the Activation of Nuclear Factor-κB-inducing Kinase and p38 Mitogen-activated Protein Kinase", Journal of Biological Chemistry, vol. 284, pp. 4439-4450, 2009. http://dx.doi.org/10.1074/jbc.M805546200
- H. Ding, G. Zhang, K.W.T. Sin, Z. Liu, R. Lin, M. Li, and Y. Li, "Activin A induces skeletal muscle catabolism via p38β mitogen‐activated protein kinase", Journal of Cachexia, Sarcopenia and Muscle, vol. 8, pp. 202-212, 2016. http://dx.doi.org/10.1002/jcsm.12145
- G. Zhang, and Y. Li, "p38β MAPK upregulates atrogin1/MAFbx by specific phosphorylation of C/EBPβ", Skeletal Muscle, vol. 2, pp. 20, 2012. http://dx.doi.org/10.1186/2044-5040-2-20
- A.R. Pogozelski, T. Geng, P. Li, X. Yin, V.A. Lira, M. Zhang, J. Chi, and Z. Yan, "p38γ Mitogen-Activated Protein Kinase Is a Key Regulator in Skeletal Muscle Metabolic Adaptation in Mice", PLoS ONE, vol. 4, pp. e7934, 2009. http://dx.doi.org/10.1371/journal.pone.0007934
- V.A. Beardmore, H.J. Hinton, C. Eftychi, M. Apostolaki, M. Armaka, J. Darragh, J. McIlrath, J.M. Carr, L.J. Armit, C. Clacher, L. Malone, G. Kollias, and J.S.C. Arthur, "Generation and Characterization of p38β (MAPK11) Gene-Targeted Mice", Molecular and Cellular Biology, vol. 25, pp. 10454-10464, 2005. http://dx.doi.org/10.1128/MCB.25.23.10454-10464.2005
- G. Zhang, R. Lin, Y.T. Kwon, and Y. Li, "Signaling mechanism of tumor cell‐induced up‐regulation of E3 ubiquitin ligase UBR2", The FASEB Journal, vol. 27, pp. 2893-2901, 2013. http://dx.doi.org/10.1096/fj.12-222711
- N. Mizushima, T. Yoshimori, and Y. Ohsumi, "The Role of Atg Proteins in Autophagosome Formation", Annual Review of Cell and Developmental Biology, vol. 27, pp. 107-132, 2011. http://dx.doi.org/10.1146/annurev-cellbio-092910-154005
- M.G. Lin, and J.H. Hurley, "Structure and function of the ULK1 complex in autophagy", Current Opinion in Cell Biology, vol. 39, pp. 61-68, 2016. http://dx.doi.org/10.1016/j.ceb.2016.02.010
- M. Bach, M. Larance, D.E. James, and G. Ramm, "The serine/threonine kinase ULK1 is a target of multiple phosphorylation events", Biochemical Journal, vol. 440, pp. 283-291, 2011. http://dx.doi.org/10.1042/BJ20101894
- D.F. Egan, D.B. Shackelford, M.M. Mihaylova, S. Gelino, R.A. Kohnz, W. Mair, D.S. Vasquez, A. Joshi, D.M. Gwinn, R. Taylor, J.M. Asara, J. Fitzpatrick, A. Dillin, B. Viollet, M. Kundu, M. Hansen, and R.J. Shaw, "Phosphorylation of ULK1 (hATG1) by AMP-Activated Protein Kinase Connects Energy Sensing to Mitophagy", Science, vol. 331, pp. 456-461, 2011. http://dx.doi.org/10.1126/science.1196371
- M.J. Puppa, E.A. Murphy, R. Fayad, G.A. Hand, and J.A. Carson, "Cachectic skeletal muscle response to a novel bout of low-frequency stimulation", Journal of Applied Physiology, vol. 116, pp. 1078-1087, 2014. http://dx.doi.org/10.1152/japplphysiol.01270.2013
- G. Zhou, R. Myers, Y. Li, Y. Chen, X. Shen, J. Fenyk-Melody, M. Wu, J. Ventre, T. Doebber, N. Fujii, N. Musi, M.F. Hirshman, L.J. Goodyear, and D.E. Moller, "Role of AMP-activated protein kinase in mechanism of metformin action", Journal of Clinical Investigation, vol. 108, pp. 1167-1174, 2001. http://dx.doi.org/10.1172/JCI13505
- J. Kim, M. Kundu, B. Viollet, and K. Guan, "AMPK and mTOR regulate autophagy through direct phosphorylation of Ulk1", Nature Cell Biology, vol. 13, pp. 132-141, 2011. http://dx.doi.org/10.1038/ncb2152
- A. Tanaka, Y. Jin, S. Lee, M. Zhang, H.P. Kim, D.B. Stolz, S.W. Ryter, and A.M.K. Choi, "Hyperoxia-Induced LC3B Interacts with the Fas Apoptotic Pathway in Epithelial Cell Death", American Journal of Respiratory Cell and Molecular Biology, vol. 46, pp. 507-514, 2012. http://dx.doi.org/10.1165/rcmb.2009-0415OC
- T. Tsukahara, Y. Matsuda, Y. Usui, and H. Haniu, "Highly purified, multi-wall carbon nanotubes induce light-chain 3B expression in human lung cells", Biochemical and Biophysical Research Communications, vol. 440, pp. 348-353, 2013. http://dx.doi.org/10.1016/j.bbrc.2013.09.089
- C. Mammucari, G. Milan, V. Romanello, E. Masiero, R. Rudolf, P. Del Piccolo, S.J. Burden, R. Di Lisi, C. Sandri, J. Zhao, A.L. Goldberg, S. Schiaffino, and M. Sandri, "FoxO3 Controls Autophagy in Skeletal Muscle In Vivo", Cell Metabolism, vol. 6, pp. 458-471, 2007. http://dx.doi.org/10.1016/j.cmet.2007.11.001
- M. Segatto, R. Fittipaldi, F. Pin, R. Sartori, K. Dae Ko, H. Zare, C. Fenizia, G. Zanchettin, E.S. Pierobon, S. Hatakeyama, C. Sperti, S. Merigliano, M. Sandri, P. Filippakopoulos, P. Costelli, V. Sartorelli, and G. Caretti, "Epigenetic targeting of bromodomain protein BRD4 counteracts cancer cachexia and prolongs survival", Nature Communications, vol. 8, 2017. http://dx.doi.org/10.1038/s41467-017-01645-7
- S.J. O'Keefe, J.S. Mudgett, S. Cupo, J.N. Parsons, N.A. Chartrain, C. Fitzgerald, S. Chen, K. Lowitz, C. Rasa, D. Visco, S. Luell, E. Carballo-Jane, K. Owens, and D.M. Zaller, "Chemical Genetics Define the Roles of p38α and p38β in Acute and Chronic Inflammation", Journal of Biological Chemistry, vol. 282, pp. 34663-34671, 2007. http://dx.doi.org/10.1074/jbc.M704236200
- P. Sicard, J.E. Clark, S. Jacquet, S. Mohammadi, J.S.C. Arthur, S.J. O'Keefe, and M.S. Marber, "The activation of p38alpha, and not p38beta, mitogen-activated protein kinase is required for ischemic preconditioning", Journal of Molecular and Cellular Cardiology, vol. 48, pp. 1324-1328, 2010. http://dx.doi.org/10.1016/j.yjmcc.2010.02.013
- E. Perdiguero, V. Ruiz-Bonilla, L. Gresh, L. Hui, E. Ballestar, P. Sousa-Victor, B. Baeza-Raja, M. Jardí, A. Bosch-Comas, M. Esteller, C. Caelles, A.L. Serrano, E.F. Wagner, and P. Muñoz-Cánoves, "Genetic analysis of p38 MAP kinases in myogenesis: fundamental role of p38α in abrogating myoblast proliferation", The EMBO Journal, vol. 26, pp. 1245-1256, 2007. http://dx.doi.org/10.1038/sj.emboj.7601587
- D. Palacios, C. Mozzetta, S. Consalvi, G. Caretti, V. Saccone, V. Proserpio, V.E. Marquez, S. Valente, A. Mai, S.V. Forcales, V. Sartorelli, and P.L. Puri, "TNF/p38α/Polycomb Signaling to Pax7 Locus in Satellite Cells Links Inflammation to the Epigenetic Control of Muscle Regeneration", Cell Stem Cell, vol. 7, pp. 455-469, 2010. http://dx.doi.org/10.1016/j.stem.2010.08.013
- M.A. Gillespie, F. Le Grand, A. Scimè, S. Kuang, J. von Maltzahn, V. Seale, A. Cuenda, J.A. Ranish, and M.A. Rudnicki, "p38-γ–dependent gene silencing restricts entry into the myogenic differentiation program", Journal of Cell Biology, vol. 187, pp. 991-1005, 2009. http://dx.doi.org/10.1083/jcb.200907037
- R.C. Ho, O. Alcazar, N. Fujii, M.F. Hirshman, and L.J. Goodyear, "p38γ MAPK regulation of glucose transporter expression and glucose uptake in L6 myotubes and mouse skeletal muscle", American Journal of Physiology-Regulatory, Integrative and Comparative Physiology, vol. 286, pp. R342-R349, 2004. http://dx.doi.org/10.1152/ajpregu.00563.2003
- Y. Xu, X. Liu, X. Gong, and N.T. Eissa, "Signaling pathway of autophagy associated with innate immunity", Autophagy, vol. 4, pp. 110-112, 2008. http://dx.doi.org/10.4161/auto.5225
- W. Zhong, H. Zhu, F. Sheng, Y. Tian, J. Zhou, Y. Chen, S. Li, and J. Lin, "Activation of the MAPK11/12/13/14 (p38 MAPK) pathway regulates the transcription of autophagy genes in response to oxidative stress induced by a novel copper complex in HeLa cells", Autophagy, vol. 10, pp. 1285-1300, 2014. http://dx.doi.org/10.4161/auto.28789
- T. Matsuzawa, B. Kim, A.R. Shenoy, S. Kamitani, M. Miyake, and J.D. MacMicking, "IFN-γ Elicits Macrophage Autophagy via the p38 MAPK Signaling Pathway", The Journal of Immunology, vol. 189, pp. 813-818, 2012. http://dx.doi.org/10.4049/jimmunol.1102041
- Y. Yu, S. Li, Z. Wang, J. He, Y. Ding, H. Zhang, W. Yu, Y. Shi, Z. Cui, X. Wang, Z. Wang, L. Sun, R. Zhang, H. Du, and Z. Zhu, "Interferon regulatory factor-1 activates autophagy to aggravate hepatic ischemia-reperfusion injury via the P38/P62 pathway in mice", Scientific Reports, vol. 7, 2017. http://dx.doi.org/10.1038/srep43684
- J. Moruno-Manchón, E. Pérez-Jiménez, and E. Knecht, "Glucose induces autophagy under starvation conditions by a p38 MAPK-dependent pathway", Biochemical Journal, vol. 449, pp. 497-506, 2012. http://dx.doi.org/10.1042/BJ20121122
- Y. Xu, C. Jagannath, X. Liu, A. Sharafkhaneh, K.E. Kolodziejska, and N.T. Eissa, "Toll-like Receptor 4 Is a Sensor for Autophagy Associated with Innate Immunity", Immunity, vol. 27, pp. 135-144, 2007. http://dx.doi.org/10.1016/j.immuni.2007.05.022
- E. Sterneck, L. Tessarollo, and P.F. Johnson, "An essential role for C/EBPβ in female reproduction", Genes & Development, vol. 11, pp. 2153-2162, 1997. http://dx.doi.org/10.1101/gad.11.17.2153
- N. Askari, J. Beenstock, O. Livnah, and D. Engelberg, "p38α Is Active in Vitro and in Vivo When Monophosphorylated at Threonine 180", Biochemistry, vol. 48, pp. 2497-2504, 2009. http://dx.doi.org/10.1021/bi900024v
- M. Avitzour, R. Diskin, B. Raboy, N. Askari, D. Engelberg, and O. Livnah, "Intrinsically active variants of all human p38 isoforms", The FEBS Journal, vol. 274, pp. 963-975, 2007. http://dx.doi.org/10.1111/j.1742-4658.2007.05644.x
SUPPLEMENTAL INFORMATION
![]() Download Supplemental Information
Download Supplemental Information
AUTHOR CONTRIBUTIONS
Y-PL and GZ designed experiments and wrote the manuscript. GZ, ZL, KWTS, HD, HAD, SG, YW and YW conducted experiments, analyzed data and generated figures. HM analyzed data.
ACKNOWLEDGMENTS
This study was supported by grants from National Institute of Arthritis and Musculoskeletal and Skin Diseases to Y.-P. Li (R01 AR063786 and AR067319). We thank Andrey Tsvetkov of UTHealth for helpful discussions, and David Engelberg (Hebrew University, Jerusalem, Israel) for sharing plasmids encoding the constitutively active mutants of p38 MAPK isoforms.
COPYRIGHT
© 2018

p38β MAPK mediates ULK1-dependent induction of autophagy in skeletal muscle of tumor-bearing mice by Liu et al. is licensed under a Creative Commons Attribution 4.0 International License.